What is Keratoconus?
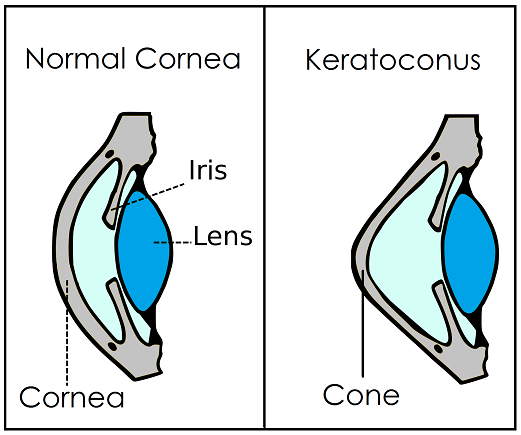
Keratoconus is a disease of the eye that begins very mild in the early decades of life and eventually requires special treatment in order to maintain vision. The disease is caused by the failure of collagen (the hard glue of the body) in the cornea to maintain its strength. As the cornea weakens, a small area of the cornea bulges forward, producing a dome or cone shape on the front of the cornea (hence the name “kerato-conus”; or cone of the cornea). Along with genetics that can lead to a weak cornea, another associated risk factor is eye rubbing, often due to allergies. Avoiding rubbing the eyes, preventing children from rubbing their eyes, and using anti-allergy eye drops are all steps that may lower risk of developing keratoconus.
What are the treatment options?
There are several treatment options for keratoconus, depending on the severity:
Mild Keratoconus
Glasses
Glasses are a poor treatment option for keratoconus and will not provide clear vision. A contact lens is almost always necessary for usable vision and is a much better option than glasses alone. A backup pair of glasses should be kept for times that contact lenses may not be worn due to health risks such as corneal ulcer, infection, or even lost lenses.
Soft Contact Lenses (Custom made)
Younger patients are able to achieve good vision with a custom made soft contact lens. In my office, we use a soft lens that is replaced every 3 months. The lens is made specifically for each patient’s eye and is usually very comfortable.
Corneal Cross-Linking
In April 2016, the FDA approved the first corneal cross-linking system in the United States. Corneal cross-linking is a procedure used to strengthen the cornea and slow the progression of early keratoconus. Ultra Violet light (UV-A) and Riboflavin (Vitamin B2) eye drops are used for the treatment, which is an outpatient procedure that generally lasts less than an hour. The procedure is not meant to improve keratoconus or cure it, but merely stabilize it. A contact lens will still be necessary to maintain vision.
Moderate Keratoconus
As the condition worsen, soft contact lenses will no longer be successful. A “hard contact lens” or RGP (Rigid gas permeable) lens is the next line of treatment. There are several different designs of RGP lenses that may be used:
Traditional RGP Lens
These lenses are small and rest directly on the cornea. They are the traditional method of correcting early-moderate keratoconus.
Scleral Contact Lens
This lens is made of the same material as an RGP, but is larger in diameter. Instead of setting on cornea, the lens rests on the sclera (white of eye). This is the preferred method of correcting moderate to moderate to severe keratoconus because it does not scar the cornea as much as traditional RGP lenses. They also may provide better comfort and vision than other types of contact lenses. Read more at my post about scleral lenses.
A backup pair of contacts is strongly recommended if vision is dependent on the contact lenses. These lenses can often take up to 1-3 weeks to order and receive, which can be devastating if relying on only one set of lenses that broke or have been lost.
Severe Keratoconus
Late stage keratoconus is detrimental to quality of life unless treated. Once scleral contact lenses no longer improve vision, cornea transplant is often the only option to increase sight. This stage of the disease is usually reached during the later decades of life and varies greatly between patients.


